By using this website, you agree to accept MoodChangeMedicine.com website’s terms of use, which can be viewed here.
April 22, 2024
By Joie Meissner, ND BCB-L
Inflammation has been implicated as an important part of the mechanism driving anxiety and depression. 1, 2, 3, 4
People with depression and anxiety have higher levels of inflammation.
Depressed people’s blood shows higher levels of pro-inflammatory markers and reductions in anti-inflammatory ones. Data spanning 5,166 depressed patients compared markers of inflammation in patients with depression with healthy controls. The researchers concluded that “Depression is confirmed as a pro-inflammatory state.” 5 Inflammation of the nervous system affects almost a third of patients with major depression who have levels noticeably higher than the majority of nondepressed individuals. 6
Increased anxiety also goes hand-in-hand with increased inflammation. A study measuring anxiety levels in healthy people showed that increased anxiety is linked to increased levels of pro-inflammatory chemicals. 7
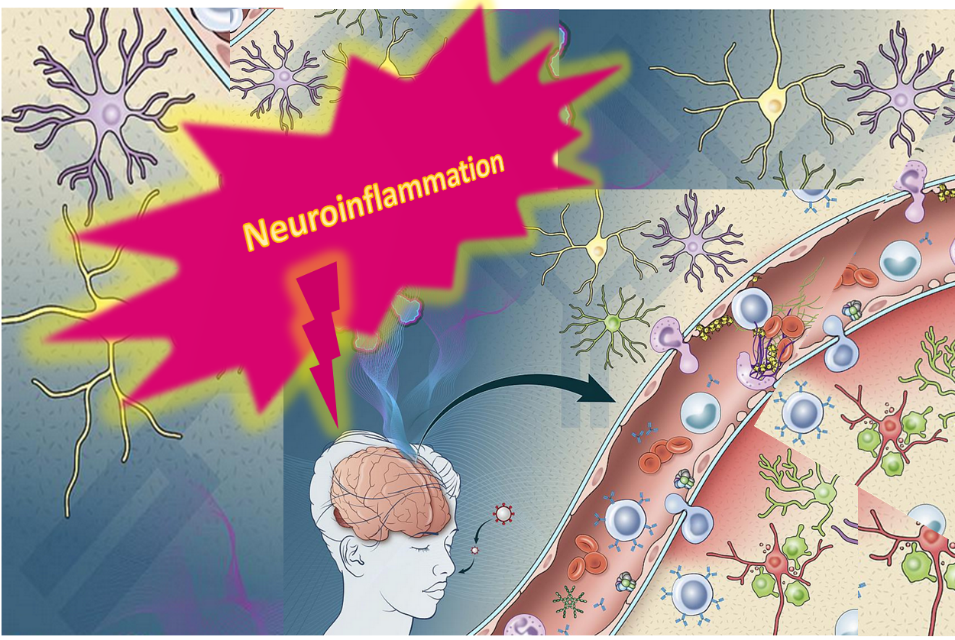
Inflammation of the nervous system affects almost a third of patients with major depression. Neuroinflammation is linked with more severe, chronic depression that can be difficult to heal with conventional treatments. 8
Studies have shown an association between inflammation and how our brains process emotional information. 9
Inflammation and its cascade of biochemical consequences including decreased neuroplasticity might be the reason that antidepressants don’t work that well in patients with high levels of inflammation. 10 And it might also explain why patients that have elevated inflammation may not respond to talk-therapy. 11
Depressed patients who start psychotherapy with higher levels of inflammation are less likely to be helped by it, a 2020 study show. And for those who had somatic symptoms of depression—like changes in appetite, fatigue, aches and pains and sleep disturbances—the worse those symptoms were, the higher the levels of inflammation. 12
If inflammation wreaks havoc on our mental and physical health, it begs the question: How?
Brain-derived neurotrophic factor (BDNF)—a biochemical force for good in our brains—is one way inflammation does its dirty work. A rise in BDNF levels stimulates the growth of new neuron cells. BDNF also stimulates nerves to make new connections with each other called synapses. The creation of new neurons and new connections between the neurons has been dubbed neuroplasticity and may play a key role in decreasing depression. BDNF-enhanced neuroplasticity has been found to rise after successful treatment of anxiety with talk therapy. 13
Inflammation significantly decreases the levels of BDNF. 14, 15
Changes in BDNF are implicated in the development of anxiety and depression via its effects on neuroplasticity of the brain. 16, 17
BDNF levels are reduced in people with major depressive disorder and increase after the depression remits. 18, 19
Scientists postulate that decreased production of BDNF contributes to depression by impairing regeneration of brain tissue. [18] Increased production of BDNF plays a role in how the brain heals from depression by facilitating regeneration of these tissues. 20 Such regeneration is a crucial aspect of neuroplasticity, which is part of the amazing resilience of the brain.
Changes in BDNF are implicated in the development of anxiety and depression via its effects on neuroplasticity of the brain. 21, 22
Neuroplasticity may also aid in the recovery from anxiety. Research on social anxiety disorder found that successful treatment improves neuroplasticity in the brain’s threat center—the part of the brain that mediates anxiety. 23
Successful treatment of social anxiety disorder was also found to reduce the size of the over-active amygdala, the brain’s threat center. 24
The ability of this brain structure—the amygdala—to reduce the size of the amygdala is an example of the amazing neuroplasticity of the brain.
Inflammation promotes anxiety and depression and losses in neuroplasticity. But what about these conditions drives inflammation in the first place?
Here are answers about how to cut stress-induced inflammation that stokes cycles of anxiety and depression. Click link below:
Care informed by the understanding that emotional and physical wellbeing are deeply connected
________________________________________________________________________________________________________________
By using this website, you agree to accept MoodChangeMedicine.com website’s terms of use, which can be viewed here.
Citations
- Cowen PJ, Browning M. “What has serotonin to do with depression?” World Psychiatry. 2015 Jun;14(2):158-60. doi: 10.1002/wps.20229. PMID: 26043325; PMCID: PMC4471964. ↩︎
- Berk M, Williams LJ, Jacka FN, O’Neil A, et al. “So depression is an inflammatory disease, but where does the inflammation come from?” BMC Med. 2013 Sep 12;11:200. doi: 10.1186/1741-7015-11-200. PMID: 24228900; PMCID: PMC3846682. ↩︎
- Pitsavos C, Panagiotakos DB, Papageorgiou C, Tsetsekou E, Soldatos C, Stefanadis C. “Anxiety in relation to inflammation and coagulation markers, among healthy adults: the ATTICA study.” Atherosclerosis. 2006 Apr;185(2):320-6. doi: 10.1016/j.atherosclerosis.2005.06.001. Epub 2005 Jul 11. PMID: 16005881 ↩︎
- Hu P, Lu Y, Pan BX, Zhang WH. “New Insights into the Pivotal Role of the Amygdala in Inflammation-Related Depression and Anxiety Disorder.” Int J Mol Sci. 2022 Sep 21;23(19):11076. doi: 10.3390/ijms231911076. PMID: 36232376; PMCID: PMC9570160. ↩︎
- Emanuele F. Osimo, Toby Pillinger, Irene Mateos Rodriguez, Golam M. Khandaker, et al. “Inflammatory markers in depression: A meta-analysis of mean differences and variability in 5,166 patients and 5,083 controls.” Brain, Behavior, and Immunity. Vol. 87,2020, Pages 901-909, doi.org/10.1016/j.bbi.2020.02.010. sciencedirect ↩︎
- Raison CL, Miller AH. “Is depression an inflammatory disorder?” Current Psychiatry Reports. 2011;13:467–475. [PMC free article] [PubMed] [Google Scholar] ↩︎
- Pitsavos C, Panagiotakos DB, Papageorgiou C, Tsetsekou E, Soldatos C, Stefanadis C. “Anxiety in relation to inflammation and coagulation markers, among healthy adults: the ATTICA study.” Atherosclerosis. 2006 Apr;185(2):320-6. doi: 10.1016/j.atherosclerosis.2005.06.001. Epub 2005 Jul 11. PMID: 16005881 ↩︎
- Hassamal, Sameer. “Chronic stress, neuroinflammation, and depression: an overview of pathophysiological mechanisms and emerging anti-inflammatories.” Front. Psychiatry. 10 May 2023. Sec. Molecular Psychiatry Volume 14 – 2023. frontiersin.psychiatry/10.3389. ↩︎
- Maydych V. “The Interplay Between Stress, Inflammation, and Emotional Attention: Relevance for Depression.” Front Neurosci. 2019 Apr 24;13:384. doi: 10.3389/fnins.2019.00384. PMID: 31068783; PMCID: PMC6491771. ↩︎
- Cowen PJ, Browning M. “What has serotonin to do with depression?” World Psychiatry. 2015 Jun;14(2):158-60. doi: 10.1002/wps.20229. PMID: 26043325; PMCID: PMC4471964. ↩︎
- Lopresti AL. “Cognitive behaviour therapy and inflammation: A systematic review of its relationship and the potential implications for the treatment of depression.” Australian & New Zealand Journal of Psychiatry. 2017;51(6):565-582. doi:10.1177/0004867417701996 ↩︎
- Strawbridge R, Marwood L, King S, et al. “Inflammatory Proteins and Clinical Response to Psychological Therapy in Patients with Depression: An Exploratory Study.” J Clin Med. 2020 Dec 2;9(12):3918. doi: 10.3390/jcm9123918. PMID: 33276697; PMCID: PMC7761611. ↩︎
- Månsson KN, Salami A, Frick A, Carlbring P, Andersson G, Furmark T, Boraxbekk CJ. “Neuroplasticity in response to cognitive behavior therapy for social anxiety disorder.” Transl Psychiatry. 2016 Feb 2;6(2):e727. doi: 10.1038/tp.2015.218. PMID: 26836415; PMCID: PMC4872422. ↩︎
- Hassamal, Sameer. “Chronic stress, neuroinflammation, and depression: an overview of pathophysiological mechanisms and emerging anti-inflammatories.” Front. Psychiatry. 10 May 2023. Sec. Molecular Psychiatry Volume 14 – 2023. frontiersin.psychiatry/10.3389. ↩︎
- Miao Z, Wang Y, Sun Z. “The Relationships Between Stress, Mental Disorders, and Epigenetic Regulation of BDNF.” Int J Mol Sci. 2020 Feb 18;21(4):1375. doi: 10.3390/ijms21041375. PMID: 32085670; PMCID: PMC7073021. ↩︎
- Kurita M, Nishino S, Kato M, Numata Y, Sato T. “Plasma brain-derived neurotrophic factor levels predict the clinical outcome of depression treatment in a naturalistic study.” PLoS One. 2012;7(6):e39212. doi: 10.1371/journal.pone.0039212. Epub 2012 Jun 27. PMID: 22761741; PMCID: PMC3384668 ↩︎
- Miao Z, Wang Y, Sun Z. “The Relationships Between Stress, Mental Disorders, and Epigenetic Regulation of BDNF.” Int J Mol Sci. 2020 Feb 18;21(4):1375. doi: 10.3390/ijms21041375. PMID: 32085670; PMCID: PMC7073021. ↩︎
- Zelada MI, Garrido V, Liberona A, Jones N, Zúñiga K, Silva H, Nieto RR. “Brain-Derived Neurotrophic Factor (BDNF) as a Predictor of Treatment Response in Major Depressive Disorder (MDD): A Systematic Review.” Int J Mol Sci. 2023 Sep 30;24(19):14810. doi: 10.3390/ijms241914810. PMID: 37834258; PMCID: PMC10572866. ↩︎
- Meng F., Liu J., Dai J., Wu M., Wang W., Liu C., et al.. (2020). “Brain-derived neurotrophic factor in 5-HT neurons regulates susceptibility to depression-related behaviors induced by subchronic unpredictable stress.” J. Psychiatr. Res. 126, 55–66. 10.1016/j.jpsychires.2020.05.003 [PubMed] [CrossRef] [Google Scholar] ↩︎
- Duman RS, Monteggia LM. “A neurotrophic model for stress-related mood disorders.” Biol Psychiatry. 2006 Jun 15;59(12):1116-27. doi: 10.1016/j.biopsych.2006.02.013. Epub 2006 Apr 21. PMID: 16631126. ↩︎
- Kurita M, Nishino S, Kato M, Numata Y, Sato T. “Plasma brain-derived neurotrophic factor levels predict the clinical outcome of depression treatment in a naturalistic study.” PLoS One. 2012;7(6):e39212. doi: 10.1371/journal.pone.0039212. Epub 2012 Jun 27. PMID: 22761741; PMCID: PMC3384668 ↩︎
- Miao Z, Wang Y, Sun Z. “The Relationships Between Stress, Mental Disorders, and Epigenetic Regulation of BDNF.” Int J Mol Sci. 2020 Feb 18;21(4):1375. doi: 10.3390/ijms21041375. PMID: 32085670; PMCID: PMC7073021. ↩︎
- Månsson KN, Salami A, Frick A, Carlbring P, Andersson G, Furmark T, Boraxbekk CJ. “Neuroplasticity in response to cognitive behavior therapy for social anxiety disorder.” Transl Psychiatry. 2016 Feb 2;6(2):e727. doi: 10.1038/tp.2015.218. PMID: 26836415; PMCID: PMC4872422 ↩︎
- Appelbaum, L.G., Shenasa, M.A., Stolz, L. et al. “Synaptic plasticity and mental health: methods, challenges and opportunities.” Neuropsychopharmacol. 48, 113–120 (2023). nature.com ↩︎



Discussion
No comments yet.