By using MoodChangeMedicine.com, you agree to accept this website’s terms of use, which can be viewed here.
May 9, 2024
By Joie Meissner ND, BCB-L
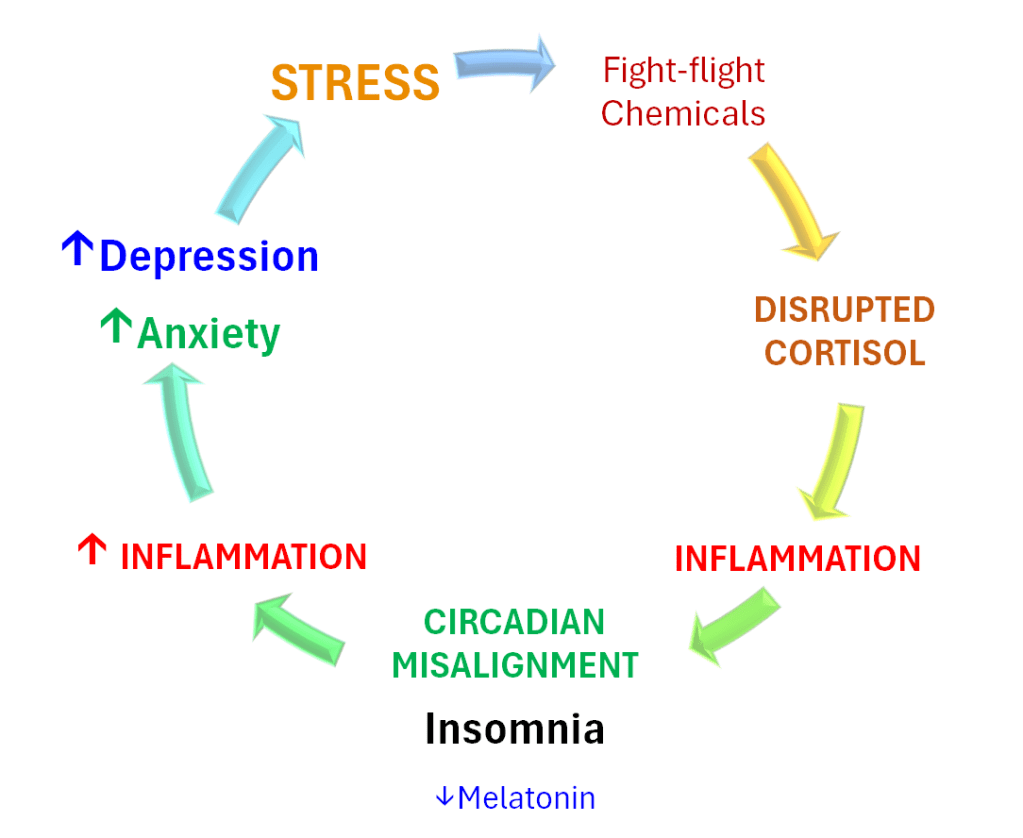
If inflammation is a bullet aimed at disrupting sleep and mental health, it’s stress that pulls the trigger. Cutting stress is a key to breaking the vicious cycle.
The stress-fed vicious cycle that causes insomnia in anxious and depressed people takes off when chronic stress triggers repeated activation of the fight-or-flight response. This repeated activation of the fight-or-flight response causes a cascade of biochemical events leading to increased inflammation that is strongly implicated in insomnia, depression, anxiety and a host of other conditions. 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11
Short-Circuiting Stress and Inflammation with Biofeedback, Hypnosis & Talk Therapy
Mood Change Medicine uses biofeedback technology to help people learn to shift out of the physiology of stress and anxiety. It helps people calm fight-or-flight physiology such as speedy hearts, anxious breathing patterns and tense muscles. These new skills build a sense of empowerment and safety. Biofeedback-Assisted Relaxation Therapy techniques include autogenic training (a form of self-hypnosis), guided imagery and progressive muscle relaxation.
Skills learned through biofeedback empower people to play an active role in self-regulating anxiety, depression, insomnia and other stress-related disorders.
Heart rate variability biofeedback not only helps to defeat stress, it has also been shown to lower cortisol levels. 12
Biofeedback-Assisted Relaxation Therapy (BART) is an important component of insomnia treatment for people with anxiety and depression. Biofeedback can be used in conjunction with cognitive behavioral therapy (CBT)—a gold-standard counseling technique used to help people overcome anxiety and depression.
Cognitive behavioral therapy has been found to reduce inflammation in 14 studies. 13 CBT reduces overactivation of the stress-responses by altering the function of a key brain structure—the amygdala—involved in setting off the fight-or-flight chemicals that trigger inflammation. 14, 15
Mood Change Medicine uses hypnotherapy, which has been found to be effective in not only lowering anxiety but also blood levels of the stress-hormone cortisol, which stokes the vicious cycle. 16, 17, 18, 19 Hypnosis has also been shown to be effective for depression. 20
Mood Change Medicine uses time-tested therapies to address biological causes of insomnia, stress, anxiety and depression including:
- Biofeedback-Assisted Relaxation Therapy (BART)
- Cognitive Behavioral Therapy for Insomnia (CBT-I)
- Transdiagnostic Sleep & Circadian Intervention (TranS-C)
- Hypnotherapy
- Polyvagal-informed therapy
- Light Therapy
- Motivational interviewing
- Diet and Nutrient Therapy
- Exercise Prescription
Resetting Biological Clocks with Cognitive-Behavioral Therapy for Insomnia
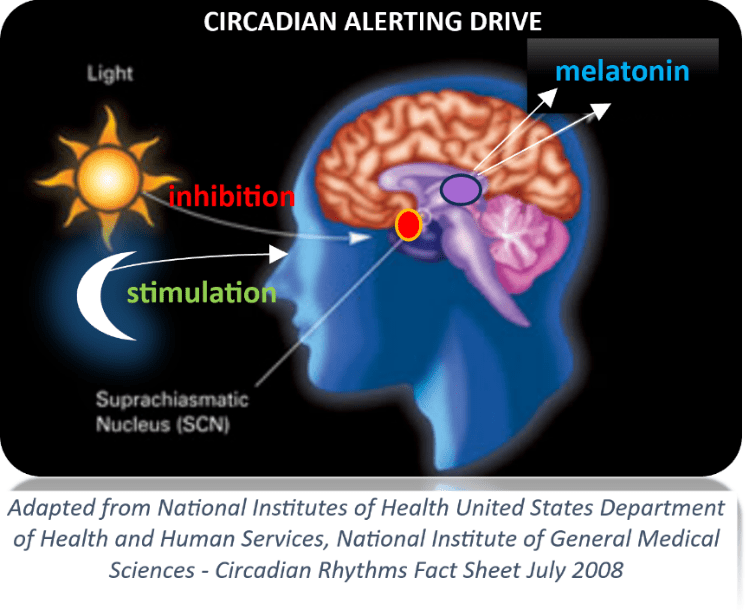
Another key to breaking the vicious cycle is normalizing circadian rhythms. Mood Change Medicine uses Cognitive-Behavioral Therapy for Insomnia (CBT-I) to restore the body’s natural sleep clock and healthy patterns of cortisol and the sleep-hormone melatonin. CBT-I, the most-recommended insomnia treatment, is the first-line treatment recommended by the American Academy of Sleep Medicine. 21
CBT-I has been shown to reduce the severity of insomnia and depression, according to a 2023 analysis of seven studies spanning 3,597 in adults diagnosed with both. The researchers concluded that it was “effective in alleviating insomnia and depression and might be considered as a viable treatment option for depression.” 22
CBT-I was found to be effective at helping people with insomnia and clinically significant anxiety symptoms by another 2023 study analyzing data from two clinical trials spanning 2,172 people. 23
Cognitive Behavioral Therapy for Insomnia (CBT-I) includes:
- Techniques to help build up the body’s natural sleep drive;
- Operant conditioning techniques based on the work of B.F. Skinner, the famous American psychologist who reshaped modern psychology;
- Sleep education, cognitive behavioral and mindfulness techniques to help break the grip of anxious thinking that interferes with sleep;
- Relaxation therapy using biofeedback (BART) to help shift the body out of fight-or-flight into a more relaxed state compatible with sleep;
- Sleep hygiene instruction to help eliminate common causes of sleeplessness; and
- Light therapy to help realign circadian rhythms of melatonin to normalize the body’s sleep clock
CBT-I as a whole—as well as individual components—are effective for insomnia and also effective for anxiety and depression.
Mindfulness-based interventions have been found to be effective for both anxiety and depression. 24
Biofeedback is part of sleep treatment programs at prestigious health care systems like Mayo Clinic in their sleep program “Insomnia treatment: Cognitive behavioral therapy instead of sleeping pills”. The Cleveland Clinic also uses biofeedback in their CBT-I program for the sleep anxiety that often accompanies insomnia.
Mood Change Medicine’s Dr. Meissner is Board Certified in Biofeedback (BCB-L) by Biofeedback Certification International Alliance.
Heart rate variability (HRV) biofeedback:
- HRV biofeedback reduced measures of depression as much as 78%, a 2016 review of research found. 25
- “HRV biofeedback training is associated with a large reduction in self-reported stress and anxiety,” a 2017 meta-analysis of 24 studies concluded. 26
Light therapy is one of the strongest ways to realign circadian rhythms such as our sleep clock:
- Light therapy has been shown to be helpful for anxiety, depression and insomnia; 27, 28, 29, 30, 31, 32
- Exposure to low levels of light, depression and insomnia can reduce melatonin levels and disrupt its circadian rhythm, which light therapy can help to restore. 33, 34 Light therapy is far more effective than melatonin supplementation alone 35, 36, 37, 38, 39, 40, 41 ; and
- Light therapy might normalize stress-triggered disruptions in the circadian rhythm of the stress-hormone cortisol that amps up anxiety, depression and insomnia 42
There are so many sources of inflammation in our lives. Inflammation triggers are ubiquitous in the indoor and outdoor environment, as well as in foods we crave.
Because we swim in a sea of inflammatory contaminants, Mood Change Medicine offers support for patients who want to curb inflammation to optimize their sleep:
- Because exercise strongly fights inflammation and certain types of exercise improve sleep quality 43, Mood Change Medicine offers help with designing an exercise program that can help boost the effectiveness of our CBT-I-based insomnia treatment program; and
- Because certain foods can fight inflammation and may also improve sleep, Mood Change Medicine offers diet and nutrient therapy that can further enhance the effectiveness of our sleep treatment program. For example:
Always consult your prescribing physician before making any changes to your medications and supplements.
If you missed the post that describes the vicious cycle of insomnia, stress, anxiety and depression and how it does its damage, click link below:
Care informed by the understanding that emotional and physical wellbeing are deeply connected
________________________________________________________________________________________________________________
By using MoodChangeMedicine.com, you agree to accept this website’s terms of use, which can be viewed here
Citations
- Dzierzewski JM, Donovan EK, Kay DB, Sannes TS, Bradbrook KE. “Sleep Inconsistency and Markers of Inflammation.” Front Neurol. 2020 Sep 16;11:1042. doi: 10.3389/fneur.2020.01042. PMID: 33041983; PMCID: PMC7525126. ↩︎
- Irwin MR, Olmstead R, Carroll JE. “Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation.” Biol Psychiatry. 2016;80:40‐52. [PMC free article] [PubMed] [Google Scholar] ↩︎
- Irwin MR, Opp MR. “Sleep Health: Reciprocal Regulation of Sleep and Innate Immunity.” Neuropsychopharmacology. 2017;42:129‐55. [PMC free article] [PubMed] [Google Scholar] ↩︎
- Irwin M.R. “Sleep and inflammation: partners in sickness and in health.” Nat. Rev. Immunol. 2019;19(11):702–715. doi: 10.1038/s41577-019-0190-z. [PubMed] [CrossRef] [Google Scholar] ↩︎
- Hassamal, Sameer. “Chronic stress, neuroinflammation, and depression: an overview of pathophysiological mechanisms and emerging anti-inflammatories.” Front. Psychiatry. 10 May 2023. Sec. Molecular Psychiatry Volume 14 – 2023. frontiersin.psychiatry/10.3389. ↩︎
- Miao Z, Wang Y, Sun Z. “The Relationships Between Stress, Mental Disorders, and Epigenetic Regulation of BDNF.” Int J Mol Sci. 2020 Feb 18;21(4):1375. doi: 10.3390/ijms21041375. PMID: 32085670; PMCID: PMC7073021. ↩︎
- Cowen PJ, Browning M. “What has serotonin to do with depression?” World Psychiatry. 2015 Jun;14(2):158-60. doi: 10.1002/wps.20229. PMID: 26043325; PMCID: PMC4471964. ↩︎
- Berk M, Williams LJ, Jacka FN, O’Neil A, et al. “So depression is an inflammatory disease, but where does the inflammation come from?” BMC Med. 2013 Sep 12;11:200. doi: 10.1186/1741-7015-11-200. PMID: 24228900; PMCID: PMC3846682. ↩︎
- Pitsavos C, Panagiotakos DB, Papageorgiou C, Tsetsekou E, Soldatos C, Stefanadis C. “Anxiety in relation to inflammation and coagulation markers, among healthy adults: the ATTICA study.” Atherosclerosis. 2006 Apr;185(2):320-6. doi: 10.1016/j.atherosclerosis.2005.06.001. Epub 2005 Jul 11. PMID: 16005881 ↩︎
- Hu P, Lu Y, Pan BX, Zhang WH. “New Insights into the Pivotal Role of the Amygdala in Inflammation-Related Depression and Anxiety Disorder.” Int J Mol Sci. 2022 Sep 21;23(19):11076. doi: 10.3390/ijms231911076. PMID: 36232376; PMCID: PMC9570160. ↩︎
- Lopresti AL. Cognitive behaviour therapy and inflammation: “A systematic review of its relationship and the potential implications for the treatment of depression.” Australian & New Zealand Journal of Psychiatry. 2017;51(6):565-582. doi:10.1177/0004867417701996 ↩︎
- Makaracı Y, Makaracı M, Zorba E, Lautenbach F. “A Pilot Study of the Biofeedback Training to Reduce Salivary Cortisol Level and Improve Mental Health in Highly-Trained Female Athletes.” Appl Psychophysiol Biofeedback. 2023 Sep;48(3):357-367. doi: 10.1007/s10484-023-09589-z. Epub 2023 May 19. PMID: 37204539. ↩︎
- Lopresti AL. “Cognitive behaviour therapy and inflammation: A systematic review of its relationship and the potential implications for the treatment of depression.” Australian & New Zealand Journal of Psychiatry. 2017;51(6):565-582. doi:10.1177/0004867417701996 ↩︎
- Appelbaum, L.G., Shenasa, M.A., Stolz, L. et al. “Synaptic plasticity and mental health: methods, challenges and opportunities.” Neuropsychopharmacol. 48, 113–120 (2023). doi.org/10.1038/s41386-022-01370-w, nature.com ↩︎
- Månsson KN, Salami A, Frick A, Carlbring P, Andersson G, Furmark T, Boraxbekk CJ. Neuroplasticity in response to cognitive behavior therapy for social anxiety disorder. Transl Psychiatry. 2016 Feb 2;6(2):e727. doi: 10.1038/tp.2015.218. PMID: 26836415; PMCID: PMC4872422. ↩︎
- Hamzah, F., Mat, K. C., & Amaran, S. (2021). “The effect of hypnotherapy on exam anxiety among nursing students.” Journal of Complementary and Integrative Medicine, 19(1), 131–137. https://doi.org/10.1515/jcim-2020-0388 PubMed Google Scholar ↩︎
- Keara E. Valentine, Leonard S. Milling, Lauren J. Clark & Caitlin L. Moriarty. “The Efficacy of Hypnosis as a Treatment for Anxiety: A Meta-Analysis.” International Journal of Clinical and Experimental Hypnosis. (2019) 67:3, 336-363, DOI: 10.1080/00207144.2019.1613863 ↩︎
- Chen PY, Liu YM, Chen ML. “The effect of hypnosis on anxiety in patients with cancer: A meta-analysis.” Worldviews Evid Based Nurs. 2017;14(3):223-236. View abstract. ↩︎
- Rizkiani, I., Respati, S. H., Sulistyowati, S., Budihastuti, U. R., & Prasetya, H. “The Effect of Hypnotherapy on Serum Cortisol Levels in Post-Cesarean Patients.” Journal of Maternal and Child Health. (2021). 6(3), 258–266. Retrieved from thejmch.com/index.php/thejmch/article/view/587 ↩︎
- Fuhr K, Meisner C, Broch A, et al. “Efficacy of hypnotherapy compared to cognitive behavioral therapy for mild to moderate depression – Results of a randomized controlled rater-blind clinical trial.” J Affect Disord. 2021;286:166-173. View abstract. ↩︎
- Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. “Clinical guideline for the evaluation and management of chronic insomnia in adults.” J Clin Sleep Med. 2008;4(5):487–504. [PMC free article] [PubMed] [Google Scholar] ↩︎
- Lin, Wenyao. Li, Na. Yang, Lili. Zhang, Yuqing. “The efficacy of digital cognitive behavioral therapy for insomnia and depression: a systematic review and meta-analysis of randomized controlled trials” PeerJ. 2023; 11: e16137. Published online 2023 Oct 31. doi: 10.7717/peerj.16137
PMID: 37927792 PMCID: PMC10624170. ↩︎ - Alasdair L. Henry, Christopher B. Miller, Richard Emsley, Bryony Sheaves, Daniel Freeman, Annemarie I. Luik, Colin A. Espie. “Does treating insomnia with digital cognitive behavioural therapy (Sleepio) mediate improvements in anxiety for those with insomnia and comorbid anxiety? An analysis using individual participant data from two large randomised controlled trials.” Journal of Affective Disorders. 2023. Vol. 339; 58-63. sciencedirect. ↩︎
- Bhattacharya, Shalini. Hofmann, Stefan G. “Mindfulness-based interventions for anxiety and depression” Clinics in Integrated Care. Vol 16, February 2023, 100138 sciencedirect.com.S2666869623000015 ↩︎
- Blase K. L., van Dijke A., Cluitmans P. J., Vermetten E. Efficacy of HRV-biofeedback as additional treatment of depression and PTSD. Tijdschrift voor Psychiatrie. 2016;58(4):292–300. [PubMed] ↩︎
- Goessl, V. C. et al. “The effect of heart rate variability biofeedback training on stress and anxiety: a meta-analysis.” Psychol Med. 2017 Nov;47(15):2578-2586. doi: 10.1017/S0033291717001003. Epub 2017 May 8. Published online by Cambridge University Press: 08 May 2017 ↩︎
- Fisher, Patrick M. et al. “Three-Week Bright-Light Intervention Has Dose-Related Effects on Threat-Related Corticolimbic Reactivity and Functional Coupling” Epub 2013 Dec 19. Biol Psychiatry. 2014 Aug 15;76(4):332-9. ↩︎
- Al-Karawi D, Jubair L. “Bright light therapy for nonseasonal depression: Meta-analysis of clinical trials.” J Affect Disord. 2016;198:64-71. View abstract. ↩︎
- Tuunainen, A., Kripke, D. F., and Endo, T. “Light therapy for non-seasonal depression.” Cochrane Database Syst Rev. 2004;(2):CD004050. View abstract. ↩︎
- Golden, R. N., Gaynes, B. N., Ekstrom, R. D., Hamer, R. M., Jacobsen, F. M., Suppes, T., Wisner, K. L., and Nemeroff, C. B. “The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence.” Am J Psychiatry. 2005;162(4):656-662. View abstract. ↩︎
- Lee TM, Chan CC. “Dose-response relationship of phototherapy for seasonal affective disorder: a meta-analysis.” Acta Psychiatr Scand. 1999 May;99(5):315-23. PMID: 10353446. View abstract. ↩︎
- van Maanen A, Meijer AM, van der Heijden KB, Oort FJ. “The effects of light therapy on sleep problems: A systematic review and meta-analysis.” Sleep Med Rev. 2016;29:52-62. View abstract. ↩︎
- von Bahr C, Ursing C, Yasui N, et al. “Fluvoxamine but not citalopram increases serum melatonin in healthy subjects – an indication that cytochrome P450 CYP1A2 and CYP2C19 hydroxylate melatonin.” Eur J Clin Pharmacol. 2000;56:123-7. View abstract. ↩︎
- Mishima K, Okawa M, Shimizu T, Hishikawa Y. “Diminished melatonin secretion in the elderly caused by insufficient environmental illumination.” J Clin Endocrinol Metab. 2001;86:129-34. View abstract. ↩︎
- Lewy AJ, Ahmed S, Jackson JM, Sack RL. “Melatonin shifts human circadian rhythms according to a phase-response curve.” Chronobiol Int. 1992;9:380-92. View abstract. ↩︎
- Zaidan, R., Geoffriau, M., Brun, J., Taillard, J., Bureau, C., Chazot, G., and Claustrat, B. “Melatonin is able to influence its secretion in humans: description of a phase-response curve.” Neuroendocrinology. 1994;60(1):105-112. View abstract. ↩︎
- Deacon, S. and Arendt, J. “Melatonin-induced temperature suppression and its acute phase-shifting effects correlate in a dose-dependent manner in humans.” Brain Res. 8-7-1995;688(1-2):77-85. View abstract. ↩︎
- Steinlechner, S. “Melatonin as a chronobiotic: PROS and CONS.” Acta Neurobiol.Exp. (Warsz.) 1996;56(1):363-372. View abstract. ↩︎
- Hatonen, T., Alila, A., and Laakso, M. L. “Exogenous melatonin fails to counteract the light-induced phase delay of human melatonin rhythm.” Brain Res. 2-26-1996;710(1-2):125-130. View abstract. ↩︎
- Cagnacci, A., Soldani, R., and Yen, S. S. “Contemporaneous melatonin administration modifies the circadian response to nocturnal bright light stimuli.” Am J Physiol. 1997;272(2 Pt 2):R482-R486. View abstract. ↩︎
- Lewy, A. J. and Sack, R. L. Exogenous melatonin’s phase-shifting effects on the endogenous melatonin profile in sighted humans: a brief review and critique of the literature. J Biol Rhythms. 1997;12(6):588-594. View abstract. ↩︎
- Fisher, Patrick M. et al. “Three-Week Bright-Light Intervention Has Dose-Related Effects on Threat-Related Corticolimbic Reactivity and Functional Coupling” Epub 2013 Dec 19. Biol Psychiatry. 2014 Aug 15;76(4):332-9. ↩︎
- Banno M, Harada Y, Taniguchi M, Tobita R, Tsujimoto H, Tsujimoto Y, Kataoka Y, Noda A. “Exercise can improve sleep quality: a systematic review and meta-analysis.” PeerJ. 2018 Jul 11;6:e5172. doi: 10.7717/peerj.5172. PMID: 30018855; PMCID: PMC6045928. ↩︎
- Jessup A, Turner-McGrievy G, Shivappa N, Hurley TG, Hébert JR. “Changes in dietary inflammatory potential predict changes in sleep quality metrics, but not sleep duration.” Sleep. 2020 Nov 12;43(11):zsaa093. doi: 10.1093/sleep/zsaa093. PMID: 32406919; PMCID: PMC7658634. ↩︎
- Losso, J. N., Finley, J. W., Karki, N., Liu, A. G., Prudente, A., Tipton, R., Yu, Y., & Greenway, F. L. “Pilot study of the tart cherry juice for the treatment of insomnia and investigation of mechanisms.” Am J Ther. 2018. Mar/Apr;25(2):e194-e201. doi: 10.1097/MJT.0000000000000584. PMID: 28901958 PMCID: PMC5617749. ↩︎
- Garrido M., Espino J., Gonzalez-Gomej D., Lozano M., Cubero J., Toribio-Delgado A.F., et al. “A Nutraceutical Product Based on Jerte Valley Cherries Improves Sleep and Augments the Antioxidant Status in Humans.” e-SPEN Eur. e-J. Clin. Nutr. Metab. 2009;4:e321–e323. doi: 10.1016/j.eclnm.2009.09.003. [CrossRef] [Google Scholar] ↩︎
- Garrido M., Gonzalez-Gomez D., Lozano M., Barriga C., Paredes S.D., Rodriguez A.B. “A Jerte valley cherry product provides beneficial effects on sleep quality.” Influence on aging. J. Nutr. Health Aging. 2013;17:553–560. doi: 10.1007/s12603-013-0029-4. [PubMed] [CrossRef] [Google Scholar] ↩︎
- Pigeon W.R., Carr M., Gorman C., Perlis M.L. “Effects of a tart cherry juice beverage on the sleep of older adults with insomnia: A pilot study.” J. Med. Food. 2010;13:579–583. doi: 10.1089/jmf.2009.0096. [PMC free article] [PubMed] [CrossRef] [Google Scholar] ↩︎
- Howatson G., Bell P.G., Tallent J., Middleton B., McHugh M.P., Ellis J. “Effect of tart cherry juice (Prunus cerasus) on melatonin levels and enhanced sleep quality.” Eur. J. Nutr. 2012;51:909–916. doi: 10.1007/s00394-011-0263-7. [PubMed] [CrossRef] [Google Scholar] ↩︎

Discussion
No comments yet.