Breaking Out of Depression: Adjunctive Therapies at Mood Change Medicine
I help people find the pathway out of pain by providing a compassionate ear using evidence-base treatments to alleviate biological causes of depression, which supports the work your doing with your psychotherapist.
Maybe it feels futile, like there’s no way out. Maybe you’re troubled by low self-esteem, guilt or regret. Maybe you’re tired of pretending to the world that everything is OK and then hiding out at home.
What is this seemingly endless parade of pain marching through your brain, stressing your mind and body? It’s the challenges of life such as illness, jobs, relationships, and loss that arise for all of us and generate ongoing stress. But it’s more than that. It’s stressed thinking, which throws gasoline on the smoldering fire of physiological stress.
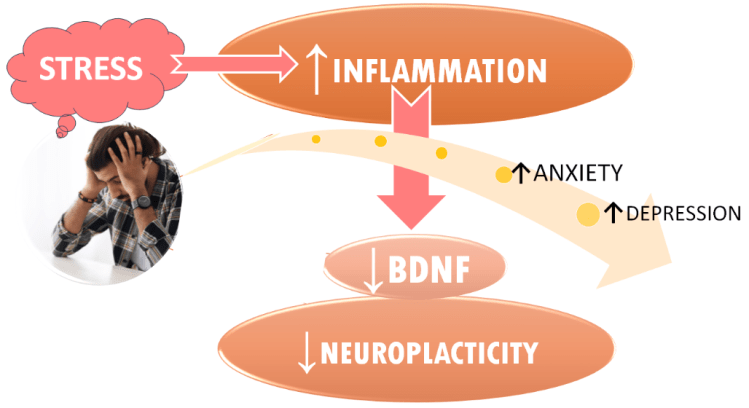
Stress is a smoking gun in the development and maintenance of depression. Science tells us that stress and the inflammation it causes are key triggers of depression. Inflammation causes physical damage to the brain and to the brain’s resiliency network that helps repair the inflammatory damage caused by stress.1, 2
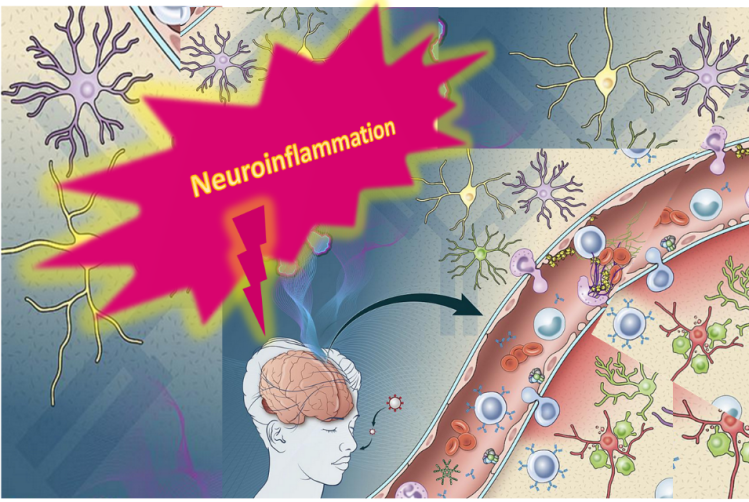
Maybe you’ve heard the phrase “it’s all in your mind.” But it’s not just all in your mind, it’s in your mind and your body. Depression is a psychological condition with a biological basis in neuroinflammation ignited by stress.
Depressed patients who start psychotherapy with higher levels of inflammation have been found to be less likely to be helped by it. And for those who had somatic symptoms of depression—like changes in appetite, fatigue, aches and pains and sleep disturbances—the worse those symptoms were, the higher the levels of inflammation. 3, 4, 5, 6
When stress strikes, it activates the fight-or-flight threat center in the brain resulting in increased inflammation causing damage to brain cells in structures responsible for mood regulation like the hippocampus. In prolonged depression, the hippocampus shrinks in size.
Inflammation causes a drop in a neurochemical called Brain-Derived Neurotrophic Factor (BDNF) and in neuroplasticity—the brain’s resiliency network. When BDNF and neuroplasticity are operating properly, they repair such inflammatory damage and depression remits. When depression is raging, BDNF plummets. When depression wanes, BDNF levels rise.
Ongoing life stressors—along with a past history of adversity, especially in childhood—shape the brain to have certain thinking patterns that can generate stress and inflammation and keep depression going in a vicious cycle. Even when external stressors diminish, depression is a self-sustaining process that generates its own stress and keeps the cycle of depression going.
When we are dealing with depression, we need tools to help manage depressive thinking patterns that generate stress and maintain the depressive cycle. Often times those thinking patterns are things we’ve experienced in early childhood that have been directing much of our subsequent behavior on an unconscious level. Some counselors call these unconscious thinking patterns that are at the center of our pain, ‘core beliefs’ or ‘schemas’. Because these thinking patterns tend to be very tenacious, depression has a way of recurring.
To prevent relapse, people need effective ways to deal with these tenacious thought patterns as well as the ongoing stress and inflammation that they generate. Part of optimal recurrence prevention includes incorporating habits that not only cut stress and inflammation but also boost the brain’s self-repair capacity.
Supplements and pharmaceuticals can’t help us manage stress effectively.
Counseling techniques like Cognitive Behavioral Therapy (CBT)—in combination with adjunctive approaches—can teach people how to dampen overactivity of the brain’s threat center, our fight-or-flight on/off switch. Drugs dampen threat centers chemically without teaching people new responses to perceived physical or social threats and any benefit disappears with drugs are discontinued. A 2024 systematic review found cognitive behavioral therapy—the gold standard for depression treatment—to be markedly more effective than drugs. 7
CBT is not the only evidence-based counseling technique but it is the most well-researched. So you may want to select a counselor who has training in CBT.
Along with standard counseling treatments for depression, an integrative approach to the treatment of depression would optimally include stress-busting therapies that address its inflammatory components as well as the sleep problems that are so common in depression.
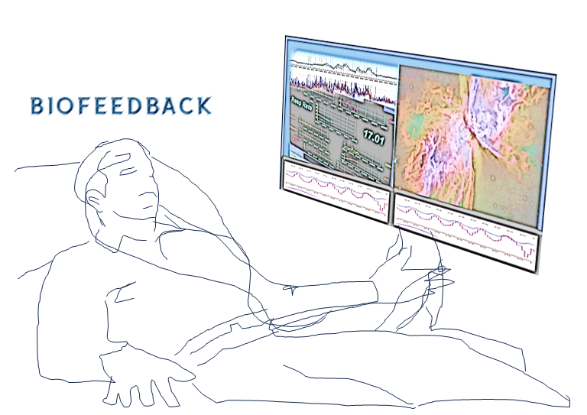
Biofeedback-Assisted Relaxation Therapy (BART) helps break the vicious cycle of stress and inflammation that stokes depression by taking the body out of fight-or-flight into a more relaxed state.
BART uses biofeedback technology to help people learn to make that shift out of the physiology of stress and into a calm state. It helps people slow speedy hearts, quiet ragged breathing patterns and relax tense muscles. These new skills build a sense of empowerment and safety. BART techniques include hypnosis, self-hypnosis, mindfulness, guided imagery and progressive muscle relaxation.
It’s quite common for people with depression to also suffer from sleep problems like insomnia, which makes depression worse. As much as 90% of people with major depression also report sleep disturbances. 8 Unfortunately, many physicians believe that when someone with depression also has insomnia, the depression should be the only focus of treatment. However, the current scientific research “provides strong evidence against the statement.” 9
In fact, when there’s insomnia in play, treatments designed to improve sleep problems, such as cognitive behavioral therapy for insomnia (CBT-I), have been shown to also improve depressive symptoms. 10
Stress disrupts the normal daily circadian rhythms of the stress-hormone cortisol and sleep-hormone melatonin. Stress spikes cortisol and lowers melatonin. This is a problem because melatonin helps put us to sleep and cortisol keeps us awake and alert. It’s a conspiracy to give us insomnia.
Stress-generated inflammation shuts down melatonin production in a brain structure called the pineal gland. 11 Melatonin—like a conductor on a passenger train—keeps the body ticking on a 24-hour clock, our circadian rhythms. Melatonin levels have been shown to decline in proportion to increases in measures of depressive symptom severity. 12, 13
Stress-spiked cortisol puts the body on alert, overriding the drive to sleep. Declining melatonin also suppresses the ability to sleep. To make matters worse insomnia and insufficient or inconsistent sleep are linked to spiking inflammation which further shut down melatonin production in the brain and can cause a vicious cycle with higher inflammation causing increasing sleeplessness. 14, 15, 16, 17
Ever wonder why when we’re depressed, we wake up in the wee hours of the morning and can’t get back to sleep? The problem is that our biological clock—our circadian rhythms—are disrupted in depression. The biological clock regulates changes in core body temperature, which normally are at their lowest early in morning. When we are depressed, we can reach the low temperature point too soon and we wake up too early. Combined with circadian disruptions in cortisol, it leaves us lying in bed mulling over problems.
A disrupted sleep clock—too much, too little or fragmented sleep—can lead to depression because circadian rhythms have a profound impact on mood.
Alterations in circadian rhythms of cortisol can impact our mood throughout the day and exacerbate the symptoms of depression. 18 A study found that depression severity was correlated with the amount of circadian misalignment: when your body’s internal clock is out of whack with the actual time of day. The more misaligned, the more severe the depressive symptoms.19
Diet and nutrition can play an integral role in mental health. There’s more than 100 million nerve cells in the gastrointestinal tract. That’s why it’s called the “second brain.” There’s a two-way communication system between the brain in our heads and the one in our guts that impacts our mood. The conversation between brain and gut is highly influenced by the billions of bacteria that line our GI tract, the microbiota. These bacteria have the ability to curb inflammation and in large part, control what nutrients we can absorb from our diet which are used to make neurotransmitters. 20, 21
“Emerging evidence shows that gut microbiota have significant roles in maintaining adequate concentrations of dopamine”—the pleasure neurotransmitter. 22
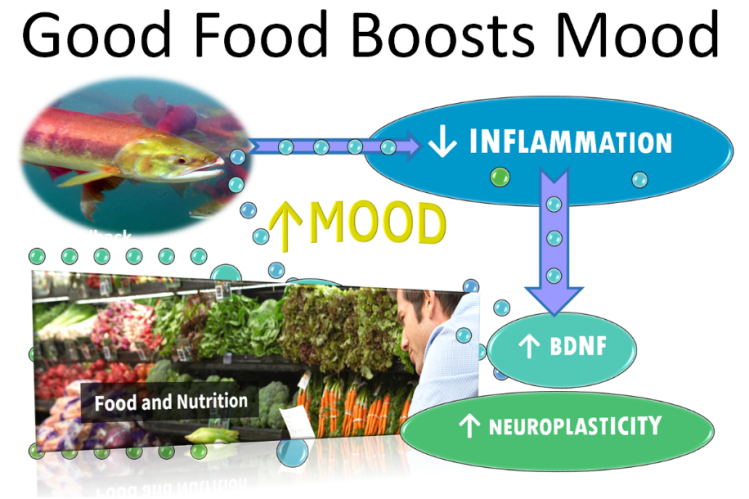
Certain foods ignite inflammation; and have been shown to increase depression risk by 45%. 23 Foods that dampen the inflammatory fire can improve depression symptoms. 24, 25
While there’s a lot of evidence in favor of eating a carefully-crafted diet with a range of anti-inflammatory foods and little or no pro-inflammatory ones, it might not be so easy for many people to design such a diet and stay on it. People can benefit from getting the expert nutrition counseling Mood Change Medicine provides.
Going on an anti-inflammatory diet improved depression in those receiving expert nutrition counseling. Thirty-two percent of the patients who got nutrition counseling achieved remission from moderate to severe depression while only 8% of the control group who received just social support did, one study found.26
People wishing to jumpstart their recovery from depression and slash their risk of recurrence may want to consider these evidence-based treatments for depression offered by Mood Change Medicine listed below:
- Biofeedback has been found to:
- Improve depression;
- Reduce stress and lower the levels of the fight-or-flight stress hormone cortisol; and
- Enhance talk therapy by acting as a bridge between our conscious awareness and our stressed physiology, allowing us to learn how to shift into a relaxed state.
Hotlink: How to De-Stress Your Way Out of Anxiety and Depression (BART)
- Hypnotherapy is a powerful enhancement to talk therapy. It has been found:
- To be as effective for mild to moderate depression as Cognitive Behavioral Therapy, the gold standard counseling treatment; and
- Lower cortisol levels, which when elevated, are an independent risk factor for depression.
Hotlink: Harness Hidden Strengths with Hypnotherapy
- Mindfulness-Based Therapies show mounting evidence of efficacy for stress, depression and anxiety:
- Mindfulness-Based Interventions can increase levels of mood-boosting BDNF, which helps repair inflammatory damage and increase neuroplasticity to heal brain tissue impacted by depression, including: mindfulness-based movement such as yoga, tai chi and qi gong.
Hotlink: Mindfulness-Based Cognitive Therapy: A Swiss-Army Knife for Tackling Anxiety & Depression
- Cognitive Behavioral Therapy for Insomnia (CBT-I) is the gold-standard treatment for insomnia recommended by the American Academy of Sleep Medicine:
- Also shown by research to be an effective depression treatment.
- CBT-I components including light therapy, biofeedback, mindfulness-based interventions and other relaxation techniques also shown in studies to improve depression.
Read more about CBT-I by clicking hotlink: Cognitive Behavioral Therapy for Insomnia
- Dietary and nutrient therapy:
- Nutritional counseling to decrease intake of inflammatory foods in favor of anti-inflammatory foods that reduce inflammation and calm its impact on neurochemistry; Depressed people who received expert diet counseling to help them follow a modified Mediterranean diet were found to achieve higher rates of remission than those in who didn’t receive diet counseling;Patients who received probiotics have shown significantly improved symptoms of depression; and
- Dietary changes and/or supplementation with certain nutrients like probiotics have been found to boost production of endogenous BDNF—the brain substance linked to better mental health, increased neuroplasticity and elevations in mood:
- High-dose EPA omega-3—a type of fish oil—can reduce inflammation, increase BDNF and may enhance the benefits of standard talk therapy treatments for depression; and
- Making dietary changes in combination with increasing exercise boosts BDNF more than exercise alone or diet alone.
Read about how probiotics improve depresssion. Hotlink: Gut-Brain Axis: Director of Mental Health?
Read how food affects mood. Hotlink: Foods that Stress and Depress—Foods that Promote Well-being
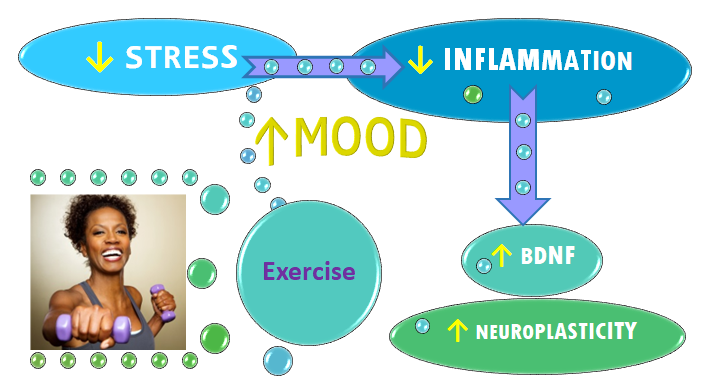
- Motivational assistance for exercise, a powerful antidepressant:
- Assisting people in getting the benefits of exercise for depression using proven behavior-change techniques like Motivational Interviewing.
- Exercise has been shown to be considerably more effective than SSRI antidepressants like Prozac, a 2024 study found.
- In countries such as Australia, exercise is recommended as “the first-line treatment approach” for mental-health conditions including depression.
- Exercise improves mental health by:
- Boosting levels of naturally-occurring, “feel-good” brain chemicals like endorphins that promote happiness and reduce stress;
- Cutting inflammation and reversing the atrophy of the hippocampus commonly found in brains of people with depression; and
- Markedly raising levels of BDNF, boosting neuroplasticity and improving depression:
- Even slow, mindfulness-based movement such as yoga, tai chi and qi gong can significantly boost BDNF levels
- Exercise fringe benefits include weight loss and improved health without potentially dangerous drug side effects
- Assisting people in getting the benefits of exercise for depression using proven behavior-change techniques like Motivational Interviewing.
Hotlink: Exercise Better than Drugs for Lifting Mood
Mood Change Medicine offers integrative therapies for insomnia & stress and adjunctive therapies for anxiety & depression.
To find out how Mood Change Medicine helps people with insomnia and depression, click link below:
To find out more about how to enhance the benefits of talk therapies for depression, click links below:
Learn more about the biological triggers of depression and how to defeat them by clicking link below:
Click link below to hear neuroscientist, Robert Sapolsky Ph.D. describe how depression is a biological disease driven by stress:
- This Stanford professor of neurology and neurosurgery shows how the parts of the brain that trigger the stress response shut down other brain areas involved in pleasure and motivation. That’s why when we’re depressed we can’t feel pleasure same as before we got depressed.
- Dr. Sapolsky explains how anxiety is linked to depression via the stress response. There are different types of depression, which cause different symptoms such as changes in energy level, sleep and appetite. He describes how changes in neurotransmitters like dopamine and serotonin can impact mood; how thyroid hormone, estrogen and especially the stress-hormone cortisol drive depression.
- He reveals how inflammation and stress ignite the biochemistry of depression and how the talk therapy, Cognitive Behavioral Therapy (CBT), helps douse the thought patterns that fuel the inflammatory fire of depression neurochemistry. He also discusses how various other types of depression treatments work.
- Sapolsky shows how depression is kindled by life experiences—psychological life stresses, especially early life stresses—which trigger depression by activating the genes that make people more vulnerable to developing depression:
Learn about nutritional supplements for depression by clicking links below:
By using this website, you agree to accept MoodChangeMedicine.com website’s terms of use, which can be viewed here.
Citations
- Sameer Hassamal, “Chronic stress, neuroinflammation, and depression: an overview of pathophysiological mechanisms and emerging anti-inflammatories.” Front. Psychiatry, 10 May 2023. Sec. Molecular Psychiatry Volume 14 – 2023 | doi.org/10.3389/fpsyt.2023.1130989 frontiersin.journals.psychiatry ↩︎
- Berk M, Williams LJ, Jacka FN, O’Neil A, et al. “So depression is an inflammatory disease, but where does the inflammation come from?” BMC Med. 2013 Sep 12;11:200. doi: 10.1186/1741-7015-11-200. PMID: 24228900; PMCID: PMC3846682. ↩︎
- Strawbridge R, Marwood L, King S, Young AH, Pariante CM, Colasanti A, Cleare AJ. “Inflammatory Proteins and Clinical Response to Psychological Therapy in Patients with Depression: An Exploratory Study.” J Clin Med. 2020 Dec 2;9(12):3918. doi: 10.3390/jcm9123918. PMID: 33276697; PMCID: PMC7761611. ↩︎
- Lopresti AL. “Cognitive behaviour therapy and inflammation: A systematic review of its relationship and the potential implications for the treatment of depression.” Australian & New Zealand Journal of Psychiatry. 2017;51(6):565-582. doi:10.1177/0004867417701996 ↩︎
- M. Maes, E. Bosmans, R. De Jongh, G. Kenis, E. Vandoolaeghe, H. Neels. “Increased serum IL-6 and IL-1 receptor antagonist concentrations in major depression and treatment resistant depression.” Cytokine. 9 (11) (1997), pp. 853-858 ↩︎
- S.M. O’Brien, P. Scully, P. Fitzgerald, L.V. Scott, T.G. Dinan. “Plasma cytokine profiles in depressed patients who fail to respond to selective serotonin reuptake inhibitor therapy.” J. Psychiatric Res. 41 (3–4) (2007), pp. 326-331 ↩︎
- Noetel M, Sanders T, Gallardo-Gómez D, Taylor P, del Pozo Cruz B, van den Hoek D et al. “Effect of exercise for depression: systematic review and network meta-analysis of randomised controlled trials.” BMJ. 2024; 384:e075847 doi:10.1136/bmj-2023-075847 ↩︎
- Franzen P.L., Buysse D.J. “Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications.” Dialogues Clin. Neurosci. 2008;10(4):473–481. doi: 10.31887/DCNS.2008.10.4/plfranzen. [PMC free article] [PubMed] [CrossRef] [Google Scholar] ↩︎
- Morin CM, Bertisch SM, Pelayo R, Watson NF, Winkelman JW, Zee PC, Krystal AD. “What Should Be the Focus of Treatment When Insomnia Disorder Is Comorbid with Depression or Anxiety Disorder?” J Clin Med. 2023 Mar 2;12(5):1975. doi: 10.3390/jcm12051975. PMID: 36902762; PMCID: PMC10004168. ↩︎
- Lin, Wenyao. Li, Na. Yang, Lili. Zhang, Yuqing. “The efficacy of digital cognitive behavioral therapy for insomnia and depression: a systematic review and meta-analysis of randomized controlled trials” PeerJ. 2023; 11: e16137. Published online 2023 Oct 31. doi: 10.7717/peerj.16137
PMID: 37927792 PMCID: PMC10624170 ↩︎ - S. da Silveira Cruz-Machado, L. Pinato, E.K. Tamura, C.E. Carvalho-Sousa, R.P. Markus. “Glia-pinealocyte network: the paracrine modulation of melatonin synthesis by tumor necrosis factor (TNF)”. PLoS One, 7 (2012), Article e40142 ↩︎
- Sundberg I, Ramklint M, Stridsberg M, Papadopoulos FC, Ekselius L, Cunningham JL. “Salivary Melatonin in Relation to Depressive Symptom Severity in Young Adults.” PLoS One. 2016 Apr 4;11(4):e0152814. doi: 10.1371/journal.pone.0152814. PMID: 27042858; PMCID: PMC4820122. ↩︎
- Souetre E, Salvati E, Belugou JL, Pringuey D, Candito M, Krebs B, et al. “Circadian rhythms in depression and recovery: evidence for blunted amplitude as the main chronobiological abnormality.” Psychiatry Res. 1989;28(3):263–78. Epub 1989/06/01. . [PubMed] [Google Scholar] ↩︎
- Dzierzewski JM, Donovan EK, Kay DB, Sannes TS, Bradbrook KE. “Sleep Inconsistency and Markers of Inflammation.” Front Neurol. 2020 Sep 16;11:1042. doi: 10.3389/fneur.2020.01042. PMID: 33041983; PMCID: PMC7525126. ↩︎
- Irwin MR, Olmstead R, Carroll JE. “Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation.” Biol Psychiatry 2016;80:40‐52. [PMC free article] [PubMed] [Google Scholar] ↩︎
- Irwin MR, Opp MR. “Sleep Health: Reciprocal Regulation of Sleep and Innate Immunity.” Neuropsychopharmacology. 2017;42:129‐55. [PMC free article] [PubMed] [Google Scholar] ↩︎
- Ballesio A. “Inflammatory hypotheses of sleep disturbance – depression link: Update and research agenda.” Brain Behav Immun Health. 2023 Jun 22;31:100647. doi: 10.1016/j.bbih.2023.100647. PMID: 37408788; PMCID: PMC10319168. ↩︎
- Boyce, Philip, Barriball, Erin. “Circadian rhythms and depression.” Australian Family Physician. Vol. 39, Issue 5, May 2010. AFP. ↩︎
- Emens J, Lewy A, Kinzie JM, Arntz D, Rough J. “Circadian misalignment in major depressive disorder.” Psychiatry Res. 2009;168(3):259–61. 10.1016/j.psychres.2009.04.009 . [PubMed] [CrossRef] [Google Scholar] ↩︎
- Kan Gao, Chun-long Mu, Aitak Farzi, Wei-yun Zhu. “Tryptophan Metabolism: A Link Between the Gut Microbiota and Brain.” Advances in Nutrition. 2020. Vol. 11, Issue 3, 2020, Pages 709-723, ISSN 2161-8313, https://doi.org/10.1093/advances/nmz127. (sciencedirect.com ) ↩︎
- Gao K, Pi Y, Mu CL, Farzi A, Liu Z, Zhu WY. “Increasing carbohydrate availability in the hindgut promotes hypothalamic neurotransmitter synthesis: aromatic amino acids linking the microbiota-brain axis.” J Neurochem. 149 (5) (2019), pp. 641-659 ↩︎
- Hamamah S, Aghazarian A, Nazaryan A, Hajnal A, Covasa M. “Role of Microbiota-Gut-Brain Axis in Regulating Dopaminergic Signaling.” Biomedicines. 2022 Feb 13;10(2):436. doi: 10.3390/biomedicines10020436. PMID: 35203645; PMCID: PMC8962300. ↩︎
- Li X, Chen M, Yao Z, Zhang T, Li Z. “Dietary inflammatory potential and the incidence of depression and anxiety: a meta-analysis.” J Health Popul Nutr. 2022 May 28;41(1):24. doi: 10.1186/s41043-022-00303-z. PMID: 35643518; PMCID: PMC9148520. ↩︎
- Jacka FN, O’Neil A, Opie R, Itsiopoulos C, Cotton S, Mohebbi M, et al. “A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’trial).” BMC Med. (2017) 15:1–13. 10.1186/s12916-017-0791-y [PMC free article] [PubMed] [CrossRef] [Google Scholar] ↩︎
- Wani AL, Bhat SA, Ara A. “Omega-3 fatty acids and the treatment of depression: a review of scientific evidence.” Integr Med Res. 2015 Sep;4(3):132-141. doi: 10.1016/j.imr.2015.07.003. Epub 2015 Jul 15. PMID: 28664119; PMCID: PMC5481805. ↩︎
- Jacka FN, O’Neil A, Opie R, Itsiopoulos C, Cotton S, Mohebbi M, et al. “A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’trial).” BMC Med. (2017) 15:1–13. 10.1186/s12916-017-0791-y [PMC free article] [PubMed] [CrossRef] [Google Scholar] ↩︎













Comments are closed.