
Calming Stress & Anxiety: Integrative & Adjunctive Therapies at Mood Change Medicine
I provide compassionate support to help stressed and anxious people step off the treadmill of trepidation, move through the fog of fear—less constrained by caution—into a fuller life using evidence-based, integrative treatments to calm stressed biology.
Those anxious feelings of foreboding that seem to never leave can suddenly surge, taking center stage—we can’t stop thinking. Overwhelming worry takes over, compelling us to do something to prevent the dreaded thing(s) from happening. But no matter how much we try to prevent, mitigate, escape from or solve the situation—that focus of our anxiety grows larger, stealing more and more of our serenity. Stress and anxiety can become a leviathan squandering the preciousness of each moment, making it hard for us to do what we need to do and to get what we want out of life.
Sometimes it’s about our fear of looking awkward in front of other people judging us. Sometimes it is fear about many things: like job responsibilities, family health, public speaking, chores we need to accomplish or going to the doctor. And sometimes we cannot figure out the specific issue to which the fear is attached. Stress seems to be swirling around us waiting for the next shoe to drop. No matter its source, our fear is part of the body’s threat-protection system designed to keep us safe from danger. The problem is that this system can run amok.
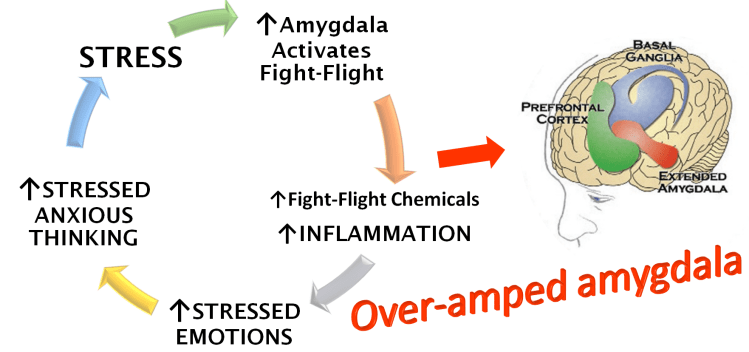
There’s an almond-shaped structure in the brain that switches on the biology of stress and anxiety—increasing heart rate, quickening breathing and elevating muscles tension—priming us for a fight or for flight. This sentinel at the center of the body’s threat system whose job it is to keep us safe from threats is called the amygdala.
When we live with chronic stress, the amygdala goes on overdrive, spawning anxiety.
“Emerging evidence suggests that the hyperactivity of amygdala neurons is a fundamental cause of chronic stress-induced anxiety disorder and depression,” scientists from the Laboratory of Fear and Anxiety Disorders explain. In this state of hyperactivity, the amygdala grows in size.1
Chronic stress causes chronic inflammation and can be very damaging to mental and physical health. Chronic stress does damage through repeated activation of the fight-or-flight biology of the body called the HPA axis, or hypothalamic-pituitary-adrenal axis. This causes a cascade of biochemical events leading to hyperactivation of inflammatory proteins that are linked to anxiety, depression and a host of other conditions. 2,3,4,5,6
Increased inflammation goes hand-in-hand with increased anxiety. A study measuring anxiety levels in healthy people showed that increased anxiety is linked to increased levels of pro-inflammatory proteins.7
Stress, stressed thinking and the inflammation they cause are at the heart of a vicious cycle of repeated activation of the amygdala. Stress and stressed thinking trigger the amygdala to turn on the fight-flight threat system that protects us from danger. The fight-or-flight system causes the release of fight-or-flight chemicals like cortisol and adrenaline. These chemicals spur inflammation in the brain and body. Once inflammation gets going, it puts the amygdala on high-alert so it is more attuned to detect signs of danger and hence more sensitive to stress. When the amygdala enters high-alert status, it ramps up our body’s fight-or-flight biology sparking an upsurge in anxious feelings and sensations. This powers anxious thinking.
As the amygdala gets continually reactivated, more and more fight-or-flight chemicals flood the system leading to a further increase in inflammation. The higher the levels of inflammation in the brain, the more sensitive the amygdala becomes to stressors, which it sees as potential threats to safety. It becomes increasingly more reactive—more easily activated so that even minor stressors can amp up anxiety. Things that weren’t causing anxiety before now trigger us. As the amygdala is hit by ever increasing levels of inflammation, it amplifies an ever-spiraling vicious cycle of anxious thinking and feelings—which are more easily set into motion by constantly living in fight-or-flight.
We can end up with a hyperactive, over-amped amygdala that can react to even the tiniest of stressors as we become ensnared in unrelenting, escalating cycles of stress, inflammation and anxiety.
Mood Change Medicine offers therapies intended to break the vicious cycle of stress and inflammation at several levels. And we provide adjunctive treatments that work synergistically to enhance the effectiveness of the psychotherapy you’re doing with your counselor.
Stressed, anxious thoughts are both the products of the vicious cycle and a fuel for it. Cognitive Behavioral Therapy (CBT) in combination with integrative approaches teaches skills that help douse the flames of inflammation by helping us step back from anxious thinking patterns. CBT has been found to reduce both the size of the amygdala and its hyperactivity in people with anxiety. Researchers postulated that these reductions in the amygdala resulted in people having less reactivity to anxiety-provoking situations. 8,9
The Laboratory of Fear and Anxiety Disorders scientists explain: “Neuroimaging studies have shown that amygdala activation in patients with anxiety disorders is significantly higher than that in controls in response to the same stimulus, which is decreased after effective cognitive behavioral therapy.”10
When the amygdala is ramped down, inflammation should theoretically be reduced because of the reduction in overactivation of the fight-or-flight chemicals that trigger it. Indeed, cognitive behavioral therapy has been found to reduce inflammation in 14 studies. 11
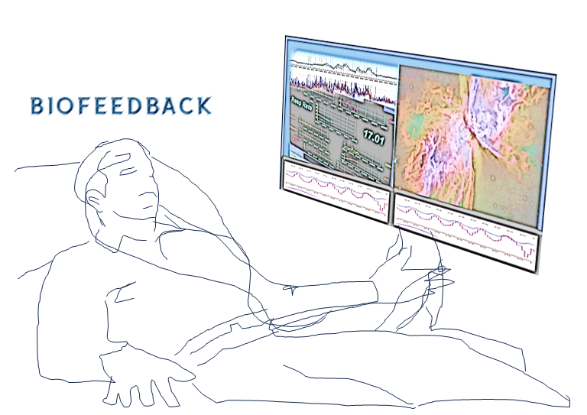
While cognitive behavioral therapy targets the thinking patterns that drive stress-inducing inflammation, Biofeedback Assisted Relaxation Therapy (BART) targets other key points in the vicious cycle. By helping us learn how to ramp down fight-or-flight physiology, BART turns down the volume of that cascade of fight-or flight chemicals, like cortisol, and adrenaline that amp up inflammation. As we shift out of fight-or-flight, our bodies feel calmer and more relaxed, which reduces anxious feelings. If your body is calm, it contradicts anxious thoughts, making them seem less threatening. By reducing daily stress levels, BART can help take the amygdala off high alert so it is not on hair-trigger resulting in heightened anxiety.
BART uses biofeedback technology to help people learn to shift out of the physiology of stress and anxiety into a calm state. It helps people slow speedy hearts, quiet anxious breathing patterns and relax tense muscles. These new skills build a sense of empowerment and safety. BART techniques include hypnosis, self-hypnosis, mindfulness, guided imagery and progressive muscle relaxation.
It’s quite common for people with anxiety to also suffer from sleep problems like insomnia, which makes anxiety worse. Unfortunately, many physicians believe that when someone with anxiety also has insomnia, the anxiety should be the only focus of treatment. However, the current scientific research “provides strong evidence against the statement.” 12
Insomnia and insufficient or inconsistent sleep are linked to spikes in the stress-hormone cortisol 13 and in inflammation. 14,15,16 Research shows that insomnia triggers anxious feelings and might cause anxiety disorders.17 Successful treatment of insomnia using cognitive behavioral therapy for insomnia (CBT-I) has been found to reduce daytime anxiety symptoms. 18
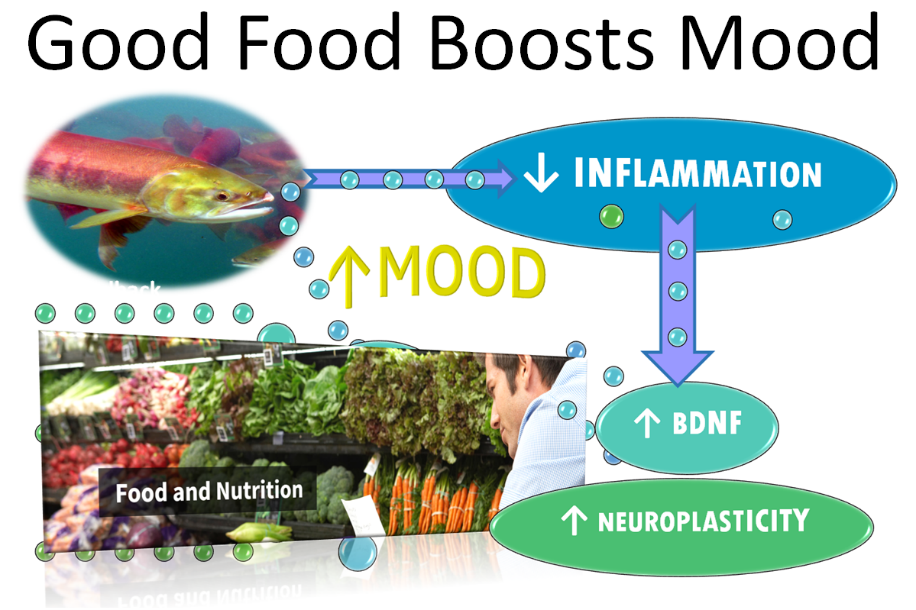
Diet and nutrition can play an integral role in mental health.
Certain foods ignite inflammation and have been shown to increase the risk of anxiety by 66%. An analysis of the results of this 2022 study looking just at women found their chances of getting anxiety was increased by 80%. Other foods dampen the inflammatory fire and can lower anxiety risk.
While there’s a lot of evidence in favor of eating a carefully-crafted diet with a range of anti-inflammatory foods and little or no pro-inflammatory ones, it might not be so easy for many people to design such a diet and stay on it without support.
People wishing to jumpstart their recovery from anxiety and slash their risk of recurrence may want to consider these evidence-based treatments for anxiety offered by Mood Change Medicine listed below:
- Biofeedback has been found to:
- Be effective at reducing levels of stress, anxiety and depressive thinking while increasing relaxation.Lower levels of the fight-or-flight stress hormone cortisol;
- Enhance talk therapy by acting as a bridge between our conscious awareness and our stressed physiology, allowing us to learn how to shift into a relaxed state.
Hotlink: How to De-Stress Your Way Out of Anxiety and Depression (BART)
- Hypnotherapy is a powerful enhancement to talk therapy. It also has been found to:
- Lower levels of the stress hormone cortisol;
- Induce a state of deep relaxation; and
- have an immediate, sustained and large effect on anxiety.
Hotlink: Harness Hidden Strengths with Hypnotherapy
- Cognitive Behavioral Therapy for Insomnia (CBT-I) is the American Academy of Sleep Medicine’s gold-standard treatment for insomnia, which is both a trigger and a symptom of anxiety:
- CBT-I can reduce anxiety symptoms, improve functioning and quality of life;
- CBT-I helps people to ramp down bedtime anxiety that keeps them tossing and turning; and
- CBT-I components include light therapy, biofeedback, mindfulness-based interventions and other relaxation techniques which also reduce anxiety.
Read more about CBT-I by clicking hotlink: Cognitive Behavioral Therapy for Insomnia
- Dietary and Nutrient Therapy:
- Switching from a diet high in inflammatory foods to an anti-inflammatory diet to reduce inflammation and calm inflammatory impact on neurochemistry;
- Mediterranean diet is an anti-inflammatory diet emphasizing olive oil, fruits, vegetables and fish that could lower the risk of anxiety.
- Reducing inflammatory-fat and ultra-processed foods in the diet, which increase anxiety;
- Dietary changes and/or supplementation with certain nutrients like probiotics have been shown to:
- Improve the health of the gut microbiota, which has been implicated in anxiety and depression.
- Boost production of endogenous BDNF—the brain substance linked to better mental health.
- Switching from a diet high in inflammatory foods to an anti-inflammatory diet to reduce inflammation and calm inflammatory impact on neurochemistry;
Read more about how probiotics improve anxiety. Hotlink: Gut-Brain Axis: Director of Mental Health?
Read how food affects mood. Hotlink: Foods that Stress and Depress—Foods that Promote Well-being
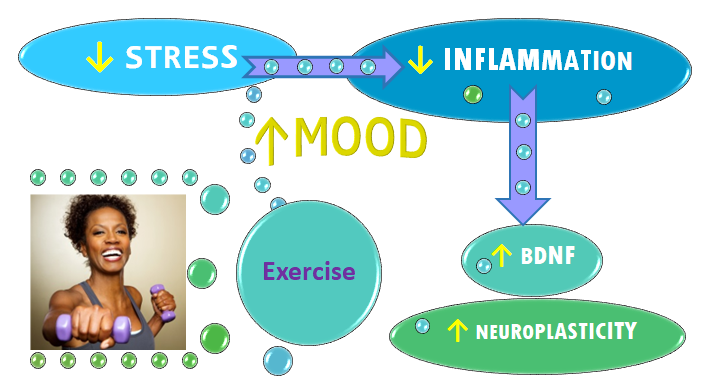
- Motivational assistance for exercise, a powerful anxiolytic:
- Assisting people in getting the benefits of exercise for anxiety using proven behavior-change techniques like Motivational Interviewing.
- Data shows exercise is a viable option for treating anxiety, a 2018 study shows.In countries such as Australia, exercise is recommended as “the first-line treatment approach” for mental-health conditions including anxiety.Exercise improves mental health by:
- Cutting inflammation; and Boosting neuroplasticity and improving anxiety:
- Exercise fringe benefits include weight loss and improved health without potentially dangerous drug side effects
- Data shows exercise is a viable option for treating anxiety, a 2018 study shows.In countries such as Australia, exercise is recommended as “the first-line treatment approach” for mental-health conditions including anxiety.Exercise improves mental health by:
- Assisting people in getting the benefits of exercise for anxiety using proven behavior-change techniques like Motivational Interviewing.
Hotlink: Exercise Better than Drugs for Lifting Mood
Mood Change Medicine offers integrative therapies for insomnia & stress and adjunctive therapies for anxiety & depression.
To find out how Mood Change Medicine helps people with stress, anxiety and insomnia, click link below:
Cutting stress-induced inflammation can enhance the benefits of talk therapies for stress and anxiety. To find out how and why, click links below:
Learn more about nutritional supplements for stress and anxiety by clicking links below:

By using this website, you agree to accept MoodChangeMedicine.com website’s terms of use, which can be viewed here.
Citations
- Hu P, Lu Y, Pan BX, Zhang WH. “New Insights into the Pivotal Role of the Amygdala in Inflammation-Related Depression and Anxiety Disorder.” Int J Mol Sci. 2022 Sep 21;23(19):11076. doi: 10.3390/ijms231911076. PMID: 36232376; PMCID: PMC9570160. ↩︎
- Berk M, Williams LJ, Jacka FN, O’Neil A, et al. “So depression is an inflammatory disease, but where does the inflammation come from?” BMC Med. 2013 Sep 12;11:200. doi: 10.1186/1741-7015-11-200. PMID: 24228900; PMCID: PMC3846682. ↩︎
- Cowen PJ, Browning M. “What has serotonin to do with depression?” World Psychiatry. 2015 Jun;14(2):158-60. doi: 10.1002/wps.20229. PMID: 26043325; PMCID: PMC4471964. ↩︎
- Miao Z, Wang Y, Sun Z. “The Relationships Between Stress, Mental Disorders, and Epigenetic Regulation of BDNF.” Int J Mol Sci. 2020 Feb 18;21(4):1375. doi: 10.3390/ijms21041375. PMID: 32085670; PMCID: PMC7073021. ↩︎
- Sameer Hassamal, “Chronic stress, neuroinflammation, and depression: an overview of pathophysiological mechanisms and emerging anti-inflammatories.” Front. Psychiatry, 10 May 2023. Sec. Molecular Psychiatry Volume 14 – 2023 | doi.org/10.3389/fpsyt.2023.1130989 frontiersin.journals.psychiatry ↩︎
- Strawbridge R, Marwood L, King S, Young AH, Pariante CM, Colasanti A, Cleare AJ. “Inflammatory Proteins and Clinical Response to Psychological Therapy in Patients with Depression: An Exploratory Study.” J Clin Med. 2020 Dec 2;9(12):3918. doi: 10.3390/jcm9123918. PMID: 33276697; PMCID: PMC7761611. ↩︎
- Pitsavos C, Panagiotakos DB, Papageorgiou C, Tsetsekou E, Soldatos C, Stefanadis C. “Anxiety in relation to inflammation and coagulation markers, among healthy adults: the ATTICA study.” Atherosclerosis. 2006 Apr;185(2):320-6. doi: 10.1016/j.atherosclerosis.2005.06.001. Epub 2005 Jul 11. PMID: 16005881 ↩︎
- Appelbaum, L.G., Shenasa, M.A., Stolz, L. et al. “Synaptic plasticity and mental health: methods, challenges and opportunities.” Neuropsychopharmacol. 48, 113–120 (2023). doi.org/10.1038/s41386-022-01370-w, nature.com ↩︎
- Månsson KN, Salami A, Frick A, Carlbring P, Andersson G, Furmark T, Boraxbekk CJ. Neuroplasticity in response to cognitive behavior therapy for social anxiety disorder. Transl Psychiatry. 2016 Feb 2;6(2):e727. doi: 10.1038/tp.2015.218. PMID: 26836415; PMCID: PMC4872422. ↩︎
- Hu P, Lu Y, Pan BX, Zhang WH. “New Insights into the Pivotal Role of the Amygdala in Inflammation-Related Depression and Anxiety Disorder.” Int J Mol Sci. 2022 Sep 21;23(19):11076. doi: 10.3390/ijms231911076. PMID: 36232376; PMCID: PMC9570160. ↩︎
- Lopresti AL. “Cognitive behaviour therapy and inflammation: A systematic review of its relationship and the potential implications for the treatment of depression.” Australian & New Zealand Journal of Psychiatry. 2017;51(6):565-582. doi:10.1177/0004867417701996 ↩︎
- Morin CM, Bertisch SM, Pelayo R, Watson NF, Winkelman JW, Zee PC, Krystal AD. “What Should Be the Focus of Treatment When Insomnia Disorder Is Comorbid with Depression or Anxiety Disorder?” J Clin Med. 2023 Mar 2;12(5):1975. doi: 10.3390/jcm12051975. PMID: 36902762; PMCID: PMC10004168. ↩︎
- Hanson, J. A., & Huecker, M. R. (2022, September 9). “Sleep deprivation.” In StatPearls. StatPearls Publishing. NBK547676. ↩︎
- Irwin MR, Opp MR. “Sleep Health: Reciprocal Regulation of Sleep and Innate Immunity.” Neuropsychopharmacology. 2017;42:129‐55. [PMC free article] [PubMed] [Google Scholar] ↩︎
- Irwin MR, Olmstead R, Carroll JE. “Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation.” Biol Psychiatry 2016;80:40‐52. [PMC free article] [PubMed] [Google Scholar]. ↩︎
- Dzierzewski JM, Donovan EK, Kay DB, Sannes TS, Bradbrook KE. “Sleep Inconsistency and Markers of Inflammation.” Front Neurol. 2020 Sep 16;11:1042. doi: 10.3389/fneur.2020.01042. PMID: 33041983; PMCID: PMC7525126. ↩︎
- Neckelmann, D., Mykletun, A., & Dahl, A. A. (2007). “Chronic insomnia as a risk factor for developing anxiety and depression.” Sleep. 30(7), 873–880.17682658 ↩︎
- Alasdair L. Henry, Christopher B. Miller, Richard Emsley, Bryony Sheaves, Daniel Freeman, Annemarie I. Luik, Colin A. Espie. “Does treating insomnia with digital cognitive behavioural therapy (Sleepio) mediate improvements in anxiety for those with insomnia and comorbid anxiety? An analysis using individual participant data from two large randomised controlled trials.” Journal of Affective Disorders. 2023. Vol. 339; 58-63. sciencedirect. ↩︎




Discussion
No comments yet.